Post-surgical nerve pain, also known as neuropathic pain, can be a challenging aspect of the recovery process for many individuals. Whether you've undergone spinal surgery, joint replacement, or other procedures, understanding the causes and management strategies for nerve pain is crucial for optimizing your recovery and quality of life.
Nerve pain after surgery can stem from various factors, including:
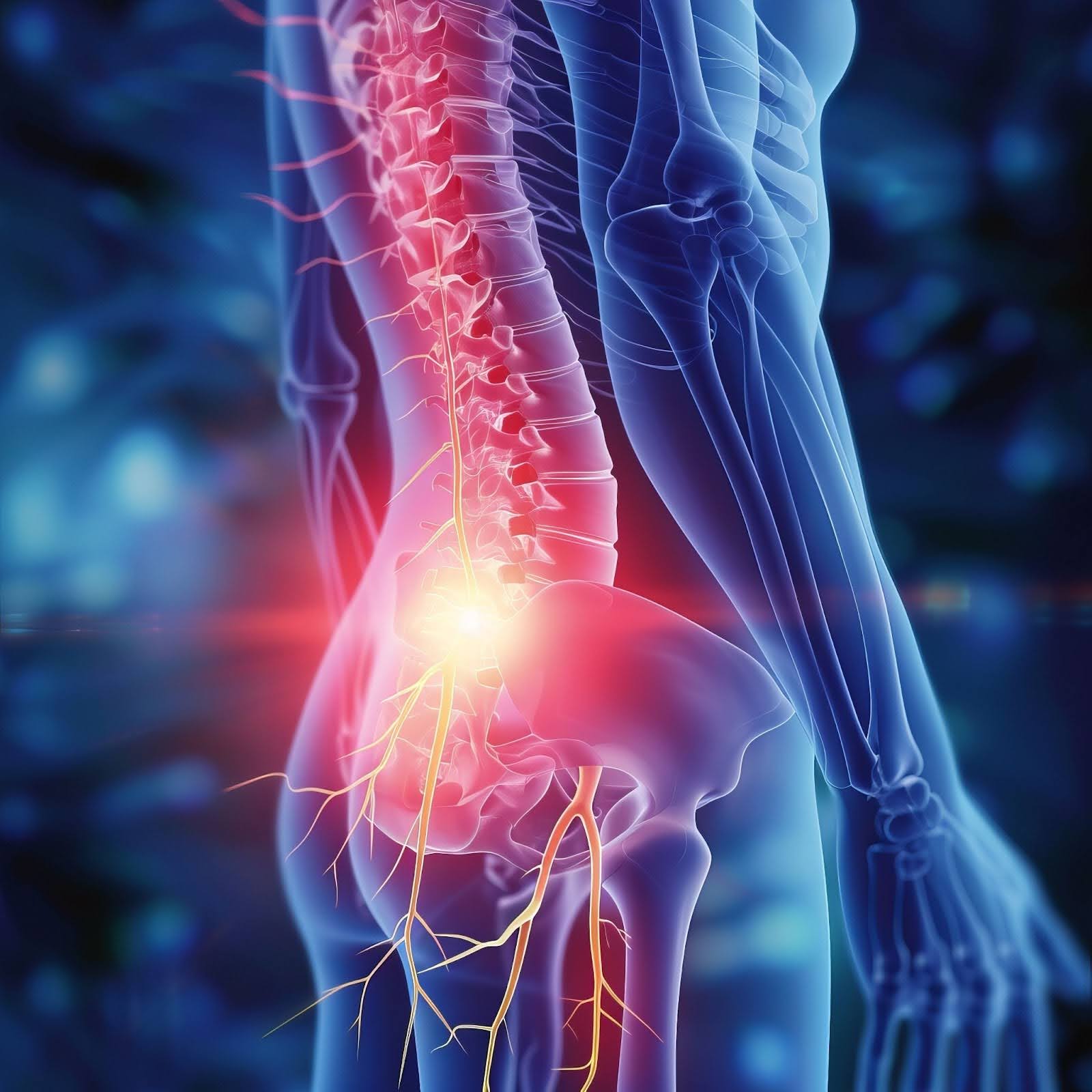
Neuropathic pain involves abnormalities in the nervous system, particularly sensitization of spinal nerves and the spinal cord. Simply put, it's like your body's pain signaling system going into overdrive, often leading to chronic pain. This phenomenon, known as central sensitization, can cause sensory abnormalities such as allodynia (non-painful stimuli perceived as painful), hyperalgesia (exaggerated pain response to painful stimuli), and radiating pain (shooting, burning, or electric-like sensations spreading from the surgery site to other areas of the body).
One of the more common types of post-surgery neuropathic pain is post laminectomy syndrome – otherwise known as pain after back surgery – but neuropathic pain can occur anywhere in the body.
Navigating post-surgical challenges involves understanding various factors contributing to nerve pain. Incomplete nerve recovery, scar tissue formation, structural alterations, recurrent disc herniation, and postoperative spinal instability all play roles in persistent discomfort, underscoring the complexity of postoperative nerve pain management.
Surgery, particularly in nerve-rich areas like the spine, can sometimes leave nerves not fully healed. These nerves act as communication wires between your body and brain. Surgeons aim to relieve pressure on them during the operation, especially if they were compressed before. But if they don't fully recover, they can continue sending pain signals to your brain, even after the initial issue is fixed. This ongoing pain is what we call nerve pain after surgery.
After surgery, scar tissue can form around the operated nerves. This scar tissue acts like a tight band, putting pressure on the nerves and causing irritation. Despite the initial problem being fixed, this ongoing irritation can lead to the nerves sending pain signals to the brain. So, in essence, nerve pain after surgery can occur because of the continued irritation caused by scar tissue pressing on the nerves.
After spine surgery, the healing process can sometimes alter the structure of your spine. Think of your spine like a stack of building blocks. If one block shifts, it can affect the stability of the entire stack. Similarly, after surgery, your spine may not return to its original shape, which can put pressure on nearby nerves. This pressure on the nerves can cause pain. So, when we mention "structural changes in the spine," we're referring to alterations in the spine's shape post-surgery, which can lead to nerve pain due to changes in nerve positioning or pressure.
Imagine your spine is like a tube filled with jelly, with layers of tough rubber bands around it to protect it. Sometimes, a part of the rubber band layer can bulge out, like a jelly donut squishing out when you press on it too hard.
Now, if you've had surgery to fix this bulging part and it happens again, it's called recurrent disc herniation. It's like the jelly squishes out again even after you've fixed it once. This can happen because the tough rubber bands might not be as strong after surgery, or because the pressure on your spine hasn't been relieved enough.
Think of your spine like a tower made of building blocks. After surgery, sometimes these blocks may not be as sturdy as they were before, which can lead to what's called postoperative spinal instability.
This instability can happen if the bones or structures in your spine aren't holding together as well as they should after surgery. It's like if some of the blocks in your tower become loose or shift out of place. This instability can put pressure on the nerves in your spine, causing pain.
Effective management of nerve pain after surgery requires a comprehensive approach tailored to individual needs. Here are some strategies to consider:
Medications: Certain medications, such as anticonvulsants, antidepressants, and neuropathic pain medications, can help alleviate nerve pain. Should be a last resort and used conservatively.
Nerve pain after surgery can significantly impact your quality of life, but with the right approach, it's possible to manage and reduce your symptoms effectively. By understanding the underlying causes of neuropathic pain and exploring various treatment options, you can take proactive steps towards a smoother recovery and improved well-being.
Remember, you're not alone in this journey.
Find a PSA location near you to receive individualized guidance and support, and don't underestimate the power of self-care and resilience in overcoming post-surgical challenges.